Product Description
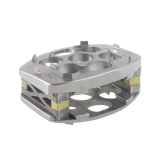
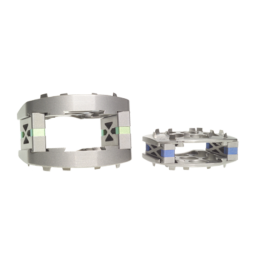
This state-of-the-art titanium spinal implant features an advanced load sharing strut design that gives the user an implant with a modulus of elasticity that mimics that of natural bone, promoting bone growth while retaining the strength of titanium. The InFix® Anterior Lumbar Device implant is assembled in situ, and provides complete sizing flexibility.
Features
- Customizable to varying patient anatomy
The modularity of the InFix device allows the user to create up to 84 different combinations of endplate size, height and lordotic angle to provide individual matching of the patient’s natural lordotic curve. - In situ assembly
InFix is assembled within the disc space, distracting as it is inserted, thereby eliminating the need to over-distract for implant insertion and thus mitigating distractor mediated endplate disruption and maintaining ligament integrity. - Sagittal balance restoration
Because no patient or pathology is the same, the InFix device was developed to help re-create the natural lordotic curvature of the spine. Different from competitive implants, the modularity of the device allows the level of lordosis to be dialed in from zero to 18 degrees.
ZS-SA0700-10_A
Device Description
The InFix device is manufactured from implantable grade Ti-6Al-4V alloy that conforms to ASTM F-136. The device is comprised of two opposing Endplates (provided in 0°, 3°, 6° and 9° angles) supported by vertical members or “Struts” available in a range of heights, allowing the surgeon to fix the vertebrae in proper anatomical alignment and lordosis. Each of the Struts includes a loadsharing mechanism that allows a limited amount of strain across the fusion mass while supporting the load bearing surfaces. An Ultra High Molecular Weight Polyethylene (UHMWPE) Endcap may be placed inside the device prior to packing it with bone graft. The Endcap effectively blocks the posterior opening in the device to contain the material inside. Holes in the Endplates provide space for bone in-growth while angled spikes penetrate the vertebral endplates and provide resistance to rotation and migration.
The InFix device is designed for direct placement between two vertebral bodies. Component sizes and dimensions are shown below. All dimensions are in millimeters. Strut heights are in 2mm increments.

 The InFix device is assembled and locked in-situ; bone graft is then inserted within the device and up to the anterior rim of the vertebral body.
The InFix device is implanted using a set of specialized instruments.
The InFix device is assembled and locked in-situ; bone graft is then inserted within the device and up to the anterior rim of the vertebral body.
The InFix device is implanted using a set of specialized instruments.
Indications
The InFix Device is a vertebral body replacement device intended for use in the thoracic and/or thoracolumbar spine (T3-L5) to replace a collapsed, damaged or unstable vertebral body resected or excised (i.e., partial or total vertebrectomy procedures) due to tumor or trauma (i.e., fracture). The InFix System is designed to restore the biomechanical integrity of the anterior, middle and posterior spinal column even in the absence of fusion for a prolonged period. The InFix Device is intended to be used with bone graft.
Contraindications
- Disease conditions which have been shown to be safely and predictably managed without the use of internal fixation devices are relative contraindications to the use of these devices.
- Active systemic infection or infection localized to the site of the proposed implantation are contraindications to implantation.
- Severe osteoporosis is a relative contraindication because it may prevent adequate fixation of spinal anchors and thus preclude the use of this or any other posterior spinal instrumentation system.
- Any entity or condition that totally precludes the possibility of fusion, i.e. cancer, kidney dialysis or osteopenia, is a relative contraindication. Other relative contraindications include obesity, pregnancy, certain degenerative disease, and foreign body sensitivity. In addition, the patient’s occupation or activity level or mental capacity may be relative contraindications to this surgery. Specifically, some patients may, because of their occupation or lifestyle, or because of conditions such as mental illness, alcoholism or drug abuse, place undue stresses on the implant.
- Known patient sensitivity to device materials (titanium alloy, Ti-6Al-4V).
- When used without posterior fixation, the device should only be used for Grade 1 or less spondylolisthesis or retrolisthesis.
Warnings
Following are specific warnings, precautions, and adverse effects, which should be understood by the surgeon and explained to the patients. These warnings do not include all adverse effects, which can occur with surgery in general, but are important considerations particular to metallic internal fixation devices. General surgical risks should be explained to the patient prior to surgery.
- THE SAFETY AND EFFECTIVENESS OF INTERBODY FUSION HAS BEEN ESTABLISHED ONLY FOR SPINAL CONDITIONS WITH SIGNIFICANT MECHANICAL INSTABILITY OR DEFORMITY REQUIRING FUSION WITH INSTRUMENTATION. These conditions are significant mechanical instability secondary to degenerative spondylolisthesis with objective evidence of neurologic impairment, fracture, dislocation, scoliosis, kyphosis, spinal tumor and failed previous fusion (pseudarthrosis). The safety and effectiveness of these devices for any other conditions is unknown. (APPLICABLE ONLY TO INDICATIONS OUTSIDE THE UNITED STATES)
- Potential risks identified with the use of this device system, which may require additional surgery, include:
- Device component fracture.
- Loss of fixation.
- Non-union.
- Fracture of the vertebra.
- Neurological injury.
- Vascular or visceral injury.
- CORRECT SELECTION OF THE IMPLANT IS EXTREMELY IMPORTANT. The potential for satisfactory fixation is increased by the selection of the proper size, shape and design of the implant. While proper selection can help minimize risks, the size and shape of human bones present limitations on the size, shape, and strength of implants. Implants height should be determined such that adequate decompression and stability are imparted to the instrumented segment.
- THE NEED FOR SUPPLEMENTAL FIXATION MUST BE DETERMINED BY THE SURGEON BASED UPON THE AMOUNT OF INSTABILITY IMPARTED BY THE SURGERY, AS WELL AS THE PATHOLOGY ITSELF. (APPLICABLE ONLY TO INDICATIONS OUTSIDE THE UNITED STATES)
- IMPLANTS CAN BREAK WHEN SUBJECTED TO THE INCREASED LOADING ASSOCIATED WITH DELAYED UNION OR NON-UNION. Internal fixation appliances are load sharing devices which are used to obtain an alignment until normal healing occurs. If healing is delayed or does not occur, the implant may eventually break due to fatigue. The degree or success of union, loads produced by weight bearing, and activity levels will, among other conditions, dictate the longevity of the implant. Notches, scratches or bending of the implant during the course of surgery may also contribute to early failure. Patients should be fully informed of the risks of implant failure.
- PATIENT SELECTION. In selecting patients for internal fixation devices, the following factors can be of extreme importance to the eventual success of the procedure:
- The patient’s weight. An overweight or obese patient can produce loads on the device that can lead to a loss of interbody height or failure of the device and/or the operation.
- The patient’s occupation or activity. If the patient is involved in an occupation or activity that includes substantial walking, running, lifting or muscle strain, the resultant forces can cause loss of disc height and/or failure of the device.
- A condition of senility, mental illness, alcoholism, or drug abuse. These conditions, among others, may cause the patient to ignore certain necessary limitations and precautions in the use of the appliance, leading to implant failure or other complications.
- Certain degenerative diseases. In some cases, the progression of degenerative disease may be so advanced at the time of implantation that it may substantially decrease the expected useful life of the appliance. For such cases, orthopaedic devices can only be considered a delaying technique or temporary relief.
- Foreign body sensitivity. Where material sensitivity is suspected, appropriate tests should be made prior to material selection or implantation.
- Smoking. Patients who smoke have been observed to experience higher rates of pseudarthrosis following surgical procedures where bone graft is used.
- These warnings do not include all adverse effects that can occur with surgery in general. General surgical risks should be explained to the patients prior to surgery.
Precautions
- THE IMPLANTATION OF SPINAL SYSTEMS SHOULD BE PERFORMED ONLY BY EXPERIENCED SURGEONS WITH SPECIFIC TRAINING IN THE USE OF SUCH SYSTEM. THIS IS A TECHNICALLY DEMANDING PROCEDURE PRESENTING A RISK OF SERIOUS INJURY TO THE PATIENT.
- SURGICAL IMPLANTS MUST NEVER BE REUSED. An explanted implant should never be reimplanted. Even though the device appears undamaged, it may have small defects and internal stress patterns that may lead to early breakage. Additional risks associated with re-use of single use devices include:
- Mechanical malfunction
- Transmission of infectious agents
- CORRECT HANDLING OF THE IMPLANT IS EXTREMELY IMPORTANT. Contouring of the metal implants should only be performed with proper equipment. The operating surgeon should avoid any notching, scratching or reverse bending of the device. Alterations will produce defects in surface finish and internal stresses which may become the focal point for eventual breakage of the implant.
- ADEQUATELY INSTRUCT THE PATIENT. Postoperative care and the patient’s ability and willingness to follow instructions are one of the most important aspects of successful bone healing. The patient must be made aware of the limitations of the implant and that physical activity and full weight bearing have been implicated in bending or fracture. The patient should understand that a metallic implant is not as strong as normal, healthy bone and will fracture if excessive demands are placed on it in the absence of complete bone healing. An active, debilitated, or demented patient who cannot properly use weight-supporting devices may be particularly at risk during postoperative rehabilitation.
Possible Adverse Effects
- Possible adverse effects associated with general surgery include complications from anesthesia, infection, hematoma and death.
- Possible adverse effects associated with laparoscopic surgery include: organ or bowel injury, peritonitis, incisional herniation, damage to blood vessels, hemorrhage, injury to the nervous system and conversion to open procedures.
- Possible adverse effects associated with gas insufflation include: hypercarbia, gas embolism, retention of gas in the peritoneum, omentum or viscera or lyphocele formation.
- Possible adverse effects associated with spinal surgery include: dural leaks, paralysis (complete or incomplete), sensory loss, loss of bowel and/or bladder control, retrograde ejaculation, failure of the bone to incorporate and scarring of nerve roots.
- Possible adverse effects associated with the InFix device may include: fracture of another vertebra during placement, device breakage, device migration, metal sensitivity or allergic reaction, spinal cord impingement, bone resorption, loss of disc height, soft tissue damage, damage to large blood vessels and pseudoarthrosis.
- Possible adverse effects associated with harvesting bone material from the iliac crest may include: pain or infection at the graft site.