Product Description
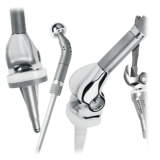
The MOST Options System is designed to enable patients facing severe bone loss of the knee or hip to regain use of their limbs and provides the potential for restoration of function.
The system goes beyond the requirements of a rotating hinge and provides the surgeon intraoperative flexibility to address a patient’s individual situation.
The anatomic, modular MOST Options System gives you maximum intraoperative flexibility in implant selection, connection, and fixation. The system offers a wide variety of implant sizes, segments, adapters, and stems to accommodate these complex cases.
The MOST Options System helps patients with problems that require surgery due to:
- Bone tumors (including benign, metastatic, and sarcoma cases)
- Revision cases requiring extensive bone resection
- Bone loss from traumatic injury
- Severe deformity such as osteomyelitis
- Damage to ligamentous supports
The Total Femoral Segment component is manufactured from Tivanium® Ti-6Al-4V Alloy and is available with or without a porous coating. It consists of a single length and 2 MOST male tapers to facilitate its use with Proximal and Distal Femoral Components and other segments.
Segments are manufactured from Ti-6Al-4V Alloy and are available in a variety of lengths to allow the surgeon to restore the leg length as closely as possible. They have a MOST male and a MOST female taper to facilitate their use with Proximal and Distal Femoral, Proximal Tibial, and I/M Stem Components and other segments.
The All-Poly Patella has an elliptical shape and is manufactured from UHMWPE.
Limb Salvage Surgery
Treatment of soft-tissue cancers of the lower limb has developed significantly over the past 30 years. Limb salvage procedures are more frequently being used to treat tumors of the lower limb. In the past, the original treatment options were limited and amputation was typically the option of choice to manage these tumors. The possibility of tumor recurrence and the possibility of metastasis limited many developments in treatment.
Advancements in chemotherapy and imaging technologies provided a door for limb salvage treatment. Chemotherapy has helped by reducing the risks associated with recurrence and metastasis. Computed tomography (CT) imaging and magnetic resonance imaging (MRI) have aided doctors by providing more detailed and precise images of tumors.
The first prostheses designed for limb salvage around the knee were constrained hinge knee systems. These first systems functioned like a door hinge and only provided extension and flexion. The constrained hinge knees had limited success and would frequently loosen. Additionally, the constrained designs could not manage rotational stress and transferred these stresses to the bone/implant interface. These stresses to the bone/implant interface were one of the key factors in early loosening for the first-generation hinged knees.
An Emphasis on Bone Preservation
The MOST Options System also offers a variety of options for attaching the implant to the bone. These options are designed to ensure that the implant is able to fit the patient’s anatomy and is well-secured. Another important feature incorporated into the MOST Options System is the resection options. The system provides bone-conserving options so bone stock can be preserved.
Cleaning Instructions
Sterility
Gamma irradiation is indicated by the symbol on the labeling. These devices remain sterile as long as the package integrity has not been violated. Inspect each package prior to use and do not use the component if any seal or cavity is damaged or breached or if the expiration date has been exceeded. Once opened, the component must be used or discarded.
Resterilization Information
These devices may not be resterilized.
Product Brochure
Indications
Contraindications
- Charcot’s joints
- Muscle deficiencies
- Multiple joint diseases
- Refusal to modify postoperative physical activities
- Obesity
- Obesity
- Heavy labor
- Active sports
- History of falls
- Use this product for other than labeled indications (off-label use)
- Use any component if damage is found or caused during setup or insertion
- Use components from other knee systems (and vice versa) unless expressly labeled for such use. Premature wear or loosening may develop and may require surgical explantation.
- Use the Tibial Revision Stem Adapter in femoral applications. It should be used only with the MOST Options Proximal Tibial Component (with or without segments).
- Impact the stem into the femoral canal after head component is assembled. Further impaction could damage the head or the Stem Adapter.
- Use the Zimmer VerSys® Hip System +10.5 Co-Cr-Mo Alloy head with the MOST Options System
- Use only the stem collet screw provided with the Hinged Femur, Hinged Tibia, and Tibial Revision Stem Adapter
- The stem collet screw has a special self-capturing feature that is designed to retain the stem should disassociation occur, and must be used with these components. No other screw should be used as a substitute
- Use only Zimmer Revision Stems of at least 190 mm in length with the MOST Options Tibial Revision Stem Adapter
- Bone screws are available for supplementary fixation as desired by the operating surgeon. These screws are not approved for attachment or fixation to the posterior elements (pedicles) of the cervical, thoracic, or lumbar spine.
- The risk of implant failure is higher with inaccurate component alignment or positioning
- Soft tissues should be balanced and components’ positioning should be confirmed
- Fat embolism risk is increased with intramedullary instrumentation and/or cement pressurization. Consider venting the femur or tibia