Product Description
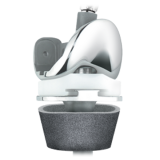
The NexGen RH Knee features a modular hinge mechanism that results in 95% of the load being carried by the tibial condyles,1 similar to the loading pattern of a primary implant design.
Because the femoral condyles remain centered on the tibia throughout the range of motion, and the shape of the patellar groove is similar to the design of the NexGen system, patella tracking is similar to a primary knee design.
For the more challenging arthroplasty procedures, the NexGen RH Knee can be used in conjunction with the Trabecular Metal™ Tibial and Femoral Cones* that address those most difficult bone-loss scenarios.
Since the NexGen RH Knee takes advantage of modular design by using NexGen Augments, the basic bone cuts are the same as those made for NexGen Primary System Components. This helps to minimize bone loss and allows use of instrumentation commonly used in primary implant procedures.
*Must be used with bone cement when used in conjunction with the NexGen RH Knee.
Patello-femoral Kinematics
The NexGen RH Knee Femoral Component has the same patello-femoral design as the other NexGen Femoral Components. The groove allows the patella to track deeply — similar to an anatomic patella. The patella is fully supported up to 60° of flexion. The central location of the hinge axis keeps the femoral condyles in a consistent sagittal plane. This allows for more normal patellar tracking since the patella does not shift posteriorly during flexion.
Designed to Limit Impact, Resist Subluxation
To resist subluxation, the NexGen RH Knee locking mechanism design offers a minimum “jump height” of 40 mm.
The ratio of conformity between the femoral condyles and the highly dished tibial articular surface is virtually 1 to 1. By maximizing contact area, the stresses in the polyethylene are distributed across a larger surface area.
Contact occurs on the frontal radius of the NexGen RH Knee Femoral Component with the articulating surface just as the implant moves to hyperextension. This will cause the knee to distract slightly, dampening the extension impact. This interaction was designed to dissipate the hyperextension force.
Pivot/Rotation
The central location of the NexGen RH Knee hinge mechanism is placed closer to the axis of the tibial component, resulting in more natural and consistent tibio-femoral kinematics when compared to posterior hinge knee designs. The rotation of theNexGen RH Knee platform is designed to displace torsional loads from the cement interfaces to the soft tissues, since it allows up to 25 degrees of movement in internal and external rotation.
Modularity of Hinge Pin/Locking Mechanism
The modularity of the hinge post extension pin allows the implantation to proceed without requiring the knee to be excessively distracted or held while the components are assembled. The NexGen RH Knee Femoral and Tibial Components are cemented into position, and, with minimal distraction, the tibial articular surface is rotated into position. The hinge post extension is easily inserted into the tibial baseplate and tightened.
95% Condylan Loading
In many conventional rotating hinge knee designs, the hinge bears the majority of the compressive load until full extension is achieved. Designs that have the center of rotation located posteriorly can cause “booking” of the joint, which may result in stress on the cement interfaces or accelerated polyethylene-bearing wear in the hinge. The NexGen RH Knee addresses these concerns as the RH Knee femoral component and articular surfaces are designed to maintain centralized contact throughout ROM (from -3° of hyperextension to 120°). The patented hinge design features passes 95% of the load through the tibial condyles.
Cleaning Instructions
Sterility
Gamma irradiation is indicated by the symbol on the labeling. These devices remain sterile as long as the package integrity has not been violated. Inspect each package prior to use and do not use the component if any seal or cavity is damaged or breached or if the expiration date has been exceeded. Once opened, the component must be used, discarded, or resterilized.
Resterilization Instructions
These sterilization instructions are consistent with ANSI/AAMI/ISO standards and guidelines. They should be used for items supplied non-sterile, for reprocessing reusable devices, or for sterile items that were opened but unused. See Zimmer booklet 97-5000-170-00 (available from your distributor) for detailed sterilization guidelines for reusable instruments and provisionals.
Solid metal implants may be resterilized only once for immediate use, in the event of inadvertent loss of sterility while preparing for surgery. This is subject to the exceptions listed below.
DO NOT RESTERILIZE
- Single-use-only components that have been contaminated with body fluids or debris or that have been previously implanted
- Trabecular Metal™ Technology components
- Components containing UHMWPE
- Components containing PMMA
Do not use the original plastic cavities or lids for resterilization. Single devices may use a standard polyethylene or Tyvek®pouch. Ensure that the pouch is large enough to contain the devices without stressing the seals or tearing the pouch.
Do not stack heavy items on top of any sterilization cases made from plastic. The resulting deformation can cause cracking of the plastic material.
Rinse porous components to remove lint or debris (using USP purified water).
Aggressive cleaning with detergents and brushes may damage special features of the implant, such as fiber metal pads or bead coatings. Also, certain detergents may be difficult to rinse off polymer items, especially those made of silicone rubber.
Items made from titanium and titanium alloys can form oxide layers from steam boiler treatment chemicals or detergent residues. While these oxides are biocompatible, they can obliterate etchings and stampings.
Modular implant components must be sterilized separately to minimize potential bioburden buildup in the dead space and expansion/contraction stresses.
Product Brochure
Indications
Individualization of Treatment
Contraindications
- This product for other than labeled indications (off-label use)
- Any component if damage is found or caused during setup or insertion
- Components from other knee systems (and vice versa) unless expressly labeled for such use. Premature wear or loosening may develop and may require surgical explantation
- Micro-sized patellas with the Rotating Hinge Knee. Excessive wear may result
- 26 or 29 mm-sized standard patellas with B, C, D, E, or F femoral components unless used in an inset mode. Excessive wear may result
- Avoid notching, scratching, or striking the device
- The potential for deep sepsis can be minimized by using biocontamination controls. Continued surveillance for new or recurrent sources of infection should be continued as long as the device is in place.
- Loosening or fracture/damage of the prosthetic knee components or surrounding tissues
- Dislocation and/or joint instability
- Malalignment of the prosthetic knee components
- Bone fracture or nerve damage
- Swelling or infection
- Leg length discrepancies
- Poor range of motion
- Pain
- Venous thromboembolic disease
- Inflammation
- Metal sensitivity
- Corrosion of metal components (the significance and long-term implications are uncertain and await further clinical evidence and evaluation)