Product Description
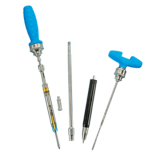
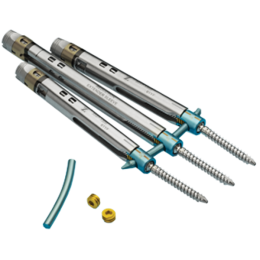
The PathFinder NXT® Minimally Invasive Pedicle Screw System is the next step forward in MIS. Backed by a legacy of clinical success with the original PathFinder® System, the PathFinder NXT System offers enhanced procedural freedom and streamlined workflow for a broad range of MIS procedures.
By offering intuitive and versatile implants and instrumentation, the Pathfinder NXT System provides spine surgeons a solution to address multiple pathologies with a less invasive approach.
Features
- Strong screw-sleeve connection prevents sleeve disassociation during surgery
- Provides up to 30mm of reduction without additional instrumentation
- Simultaneous distraction/compression and reduction allows sequential, controlled correction
- Pedicle Access Tool streamlines the pedicle targeting process and workflow
- Proprietary decortication and aspiration instruments help to facilitate a solid fusion all through the same incision
ZS-SA0700-14_A
Device Description
The Zimmer Spine PathFinder NXT system consists of polyaxial cannulated screws and rods and is intended to provide temporary stabilization following surgery to fuse the spine. A range of spinal rod lengths included with PathFinder NXTallows the surgeon to place polyaxial pedicle screws through an open or mini-open procedure.
The PathFinder NXT System is designed to aid in the surgical correction of several types of spinal conditions. This system is intended only to provide stabilization during the development of a solid fusion with autograft or allograft. These implants are intended to be removed after the development of a solid fusion mass.
The PathFinder NXT System only allows the placement of 5.5 mm titanium rods.
Indications
1. When intended for pedicle screw fixation from T1-S1, the PathFinder NXT System is intended to be used with 5.5mm rods to provide immobilization and stabilization of spinal segments in skeletally mature patients as an adjunct to fusion in the treatment of the following acute and chronic instabilities or deformities of the thoracic, lumbar and sacral spine: degenerative disc disease (defined as discogenic back pain with degeneration of the disc confirmed by history and radiographic studies), degenerative spondylolisthesis with objective evidence of neurologic impairment, fracture, dislocation, deformities or curvatures (i.e. scoliosis, kyphosis, and/or lordosis), tumor, and failed previous fusion.
2. As a pedicle screw system placed between L3 and S1, the indications for PathFinder NXT, used with 5.5mm rods, include Grade 3 or Grade 4 spondylolisthesis, when utilizing autograft or allograft, when affixed to the posterior lumbosacral spine, and is intended to be removed after solid fusion is established.
Contraindications
1. Disease conditions which have been shown to be safely and predictably managed without the use of internal fixation devices are relative contraindications to the use of these devices.
2. Active systemic infection or infection localized to the site of the proposed implantation are contraindications to implantation.
3. Severe osteoporosis is a relative contraindication because it may prevent adequate fixation of spinal anchors and thus preclude the use of this or any other posterior spinal instrumentation system.
4. Any entity or condition that totally precludes the possibility of fusion, i.e. cancer, kidney dialysis or osteopenia, is a relative contraindication. Other relative contraindications include obesity, pregnancy, certain degenerative disease, and foreign body sensitivity. In addition, the patient’s occupation or activity level or mental capacity may be relative contraindications to this surgery. Specifically, some patients may, because of their occupation or lifestyle, or because of conditions such as mental illness, alcoholism or drug abuse, place undue stresses on the implant.
Warnings
Following are specific warnings, precautions, and adverse effects that should be understood by the surgeon and explained to the patient. These warnings do not include all adverse effects that can occur with surgery in general, but are important considerations particular to metallic internal fixation devices. General surgical risks should be explained to the patient prior to surgery.
1. IN THE U.S.A., THIS PRODUCT HAS LABELING LIMITATIONS.
2. THE SAFETY AND EFFECTIVENESS OF PEDICLE SCREW SPINAL SYSTEMS HAVE BEEN ESTABLISHED ONLY FOR SPINAL CONDITIONS WITH SIGNIFICANT MECHANICAL INSTABILITY OR DEFORMITY REQUIRING FUSION WITH INSTRUMENTATION. These conditions are significant mechanical instability secondary to degenerative spondylolisthesis with objective evidence of neurologic impairment, fracture, dislocation, scoliosis, kyphosis, spinal tumor and failed previous fusion (pseudarthrosis). The safety and effectiveness of these devices for any other conditions is unknown.
3. BENEFIT OF SPINAL FUSIONS UTILIZING ANY PEDICLE SCREW FIXATION SYSTEM HAS NOT BEEN ADEQUATELY ESTABLISHED IN PATIENTS WITH STABLE SPINES. Potential risks identified with the use of this device system, which may require additional surgery, include:
a) Device component fracture.
b) Loss of fixation.
c) Non-union.
d) Fracture of the vertebra.
e) Neurological injury.
f) Vascular or visceral injury.
4. CORRECT SELECTION OF THE IMPLANT IS EXTREMELY IMPORTANT. The potential for satisfactory fixation is increased by the selection of the proper size, shape and design of the implant. While proper selection can help minimize risks, the size and shape of human bones present limitations on the size, shape, and strength of implants. Metallic internal fixation devices cannot withstand activity levels equal to those placed on normal healthy bone. No implant can be expected to withstand indefinitely the unsupported stress of full weight bearing.
5. IMPLANTS CAN BREAK WHEN SUBJECTED TO THE INCREASED LOADING ASSOCIATED WITH DELAYED UNION OR NON-UNION. Internal fixation appliances are load sharing devices which are used to obtain an alignment until normal healing occurs. If healing is delayed or does not occur, the implant may eventually break due to metal fatigue. The degree or success of union, loads produced by weight bearing, and activity levels will, among other conditions, dictate the longevity of the implant. Notches, scratches or bending of the implant during the course of surgery may also contribute to early failure. Patients should be fully informed of the risks of implant failure.
6. MIXING METALS CAN CAUSE CORROSION. There are many forms of corrosion damage and several of these occur on metals surgically implanted in humans. General or uniform corrosion is present on all implanted metals and alloys. The rate of corrosive attack on metal implant devices is usually very low due to the presence of passive surface films. Dissimilar metals in contact, such as titanium and stainless steel, accelerate the corrosion process of stainless steel and more rapid attack occurs. The presence of corrosion compounds released into the body system
will also increase. Internal fixation devices, such as rods, hooks, wires, etc. which come into contact with other metal objects, must be made from like or compatible metals.
7. PATIENT SELECTION. In selecting patients for internal fixation devices, the following 7 factors can be of extreme importance to the eventual success of the procedure:
a) The patient’s weight. An overweight or obese patient can produce loads on the
device that can lead to failure of the appliance and the operation.
b) The patient’s occupation or activity. If the patient is involved in an occupation or
activity that includes substantial walking, running, lifting or muscle strain, the
resultant forces can cause failure of the device.
c) A condition of senility, mental illness, alcoholism, or drug abuse. These
conditions, among others, may cause the patient to ignore certain necessary
limitations and precautions in the use of the appliance, leading to implant failure
or other complications.
d) Certain degenerative diseases. In some cases, the progression of degenerative
disease may be so advanced at the time of implantation that it may substantially
decrease the expected useful life of the appliance. For such cases, orthopaedic
devices can only be considered a delaying technique or temporary relief.
e) Foreign body sensitivity. Where material sensitivity is suspected, appropriate tests
should be made prior to material selection or implantation.
f) Smoking. Patients who smoke have been observed to experience higher rates of
pseudarthrosis following surgical procedures where autograft or allograft is used.
Precautions
1. THE IMPLANTATION OF PEDICLE SCREW SPINAL SYSTEMS SHOULD BE PERFORMED ONLY BY EXPERIENCED SURGEONS WITH SPECIFIC TRAINING IN THE USE OF THIS PEDICLE SCREW SPINAL SYSTEM BECAUSE THIS IS A TECHNICALLY DEMANDING PROCEDURE PRESENTING A RISK OF SERIOUS INJURY TO THE PATIENT.
2. SURGEONS SHOULD HAVE KNOWLEDGE OF HOW TO TARGET PEDICLE SCREWS USING FLUOROSCOPY AND K-WIRE WHEN UTILIZING A MINIOPEN OR PERCUTANEOUS SURGICAL TECHNIQUE.
3. SURGICAL IMPLANTS MUST NEVER BE REUSED. An explanted metal implant should never be re-implanted. Even though the device appears undamaged, it may have small defects and internal stress patterns that may lead to early breakage.
4. CORRECT HANDLING OF THE IMPLANT IS EXTREMELY IMPORTANT. Contouring of the metal implants should only be performed with proper equipment. The operating surgeon should avoid any notching, scratching or reverse bending of the devices when contouring. Alterations will produce defects in surface finish and internal stresses which may become the focal point for eventual breakage of the implant. Bending of screws will significantly decrease fatigue life and may cause failure.
5. REMOVAL OF THE IMPLANT AFTER HEALING. Metallic implants can loosen, fracture, corrode, migrate, possibly increase the risk of infection, cause pain, or stress shield bone even after healing, particularly in young, active patients. The surgeon should carefully weigh the risk versus benefits when deciding whether to remove the
implant. Implant removal should be followed by adequate postoperative management to avoid refracture. If the patient is older and has a low activity level, the surgeon may choose not to remove the implant thus eliminating the risk involved with a second surgery.
6. ADEQUATELY INSTRUCT THE PATIENT. Postoperative care and the patient’s ability and willingness to follow instructions are one of the most important aspects of successful bone healing. The patient must be made aware of the limitations of the implant and that physical activity and full weight bearing have been implicated in bending or fracture. The patient should understand that a metallic implant is not as strong as normal, healthy bone and will fracture if excessive demands are placed on it in the absence of complete bone healing. An active, debilitated, or demented patient who cannot properly use weight-supporting devices may be particularly at risk during postoperative rehabilitation.
7. “The DEVICE has not been evaluated for safety and compatibility in the MR environment. The DEVICE has not been tested for heating or migration in the MR environment.”
8. All implants and some instruments are intended for single-use only; refer to the product label to determine if the instrument is single use only. Single use devices should not be re-used. Possible risks associated with re-use of single-use devices include:
• Mechanical malfunction
• Transmission of infectious agents
Possible Adverse Effects
- Non-union, delayed union.
- Bending or fracture of implant. Fraying, kinking, loosening, bending or breaking of any or all of the cable implant components.
- Loosening of the implant.
- Metal sensitivity, or allergic reaction to a foreign body.
- Infection.
- Decrease in bone density due to stress shielding.
- Pain, discomfort, or abnormal sensations due to the presence of the device.
- Loss of proper spinal curvature, correction height and/or reduction.
- Cable cutting through soft osteoporotic, osteogenic or cancellous bone.
- Vascular and/or nerve damage due to surgical trauma or presence of the device. Neurological difficulties including bowel and/or bladder dysfunction, impotence, retrograde ejaculation, and paraesthesia.
- Bursitis.
- Dural leak.
- Paralysis.
- Death.
- Erosion of blood vessels due to the proximity of the device, leading to hemorrhage and/or death.