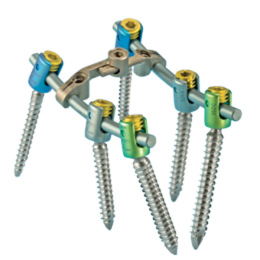
Product Description
Developed in collaboration with surgeons, the Sequoia Pedicle Screw System sets a new standard with intuitive features that simplify spine surgical flow, speed implantation, minimize head splay and provide surgeon comfort.
Features
- Screws and taps feature a double-lead thread design, expediting advancement and reducing surgeon fatigue
- Low-profile screws sit less prominently
- Helical Flange closure top technology reduces cross-threading and head splay
- Over-molded handles offer a comfortable and easy-gripping surface
- An efficient tray layout and color-coded instrumentation improve surgical flow
- Instruments are coated with Aluminum Ti Nitride, reducing reflectivity under bright lights
ZS-SA0700-18_A
Device Description
The Zimmer Spine Sequoia Pedicle Screw System is designed to aid in the surgical correction of several types of spinal conditions. This system is intended only to provide stabilization during the development of a solid fusion with a bone graft. These implants are intended to be removed after the development of a solid fusion mass.
The Sequoia Pedicle Screw System consisting of open style polyaxial screws, titanium rods (varying lengths) and connectors is intended to provide temporary stabilization following surgery to fuse the spine. The polyaxial screw design allows the surgeon to use a top-loading technique for dropping the spinal rod down to the fixation components into a u-shaped opening.
This system offers a single package containing a wide array of implant styles, allowing the surgeon maximum flexibility to address patient needs.
SpeedLink II™ Transverse Connectors are provided to increase rotational stiffness to the final construct.
Indications
When intended for pedicle screw fixation from T1-S1, the Sequoia Pedicle Screw System is intended to provide immobilization and stabilization of spinal segments in skeletally mature patients as an adjunct to fusion in the treatment of the following acute and chronic instabilities or deformities of the thoracic, lumbar, and sacral spine: degenerative disc disease (defined as discogenic back pain with degeneration of the disc confirmed by history and radiographic studies), degenerative spondylolisthesis with objective evidence of neurologic impairment, fracture, dislocation, deformities, or curvatures (i.e. scoliosis, kyphosis, and/or lordosis), tumor, and failed previous fusion. As a pedicle screw system placed between L3 and S1, the indications include Grade 3 or Grade 4 spondylolisthesis, when utilizing autologous bone graft, when affixed to the posterior lumbosacral spine, and intended to be removed after solid fusion is established. When intended for non-pedicle, posterior screw fixation of the non-cervical spine (T1- S1), the indications are idiopathic scoliosis, neuromuscular scoliosis/kyphoscoliosis with associated paralysis or spasticity, scoliosis with deficient posterior elements such as that resulting from laminectomy or myelomeningocele, spinal fractures (acute reduction or late deformity), degenerative disc disease (back pain of discogenic origin with degeneration of the disc confirmed by history and radiographic studies), tumor, spondylolisthesis, spinal stenosis, and failed previous fusion. When intended for anterolateral screw, rod, and/or cable fixation of the T6-L5 spine, the indications are degenerative disc disease (back pain of discogenic origin with degeneration of the disc confirmed by history and radiographic studies), spondylolisthesis, trauma (i.e. fracture or dislocation), spinal stenosis, deformities or curvatures (i.e. scoliosis, kyphosis, and/or lordosis), tumor, and failed previous fusion.
Contraindications
- Disease conditions which have been shown to be safely and predictably managed without the use of internal fixation devices are relative contraindications to the use of these devices.
- Active systemic infection or infection localized to the site of the proposed implantation are contraindications to implantation.
- Severe osteoporosis is a relative contraindication because it may prevent adequate fixation of spinal anchors and thus preclude the use of this or any other posterior spinal instrumentation system.
- Any entity or condition that totally precludes the possibility of fusion, i.e. cancer, kidney dialysis, or osteopenia, is a relative contraindication. Other relative contraindications include obesity, pregnancy, certain degenerative disease, and foreign body sensitivity. In addition, the patient’s occupation or activity level or mental capacity may be relative contraindications to this surgery. Specifically, some patients may, because of their occupation or lifestyle, or because of conditions such as mental illness, alcoholism or drug abuse, place undue stresses on the implant.
Warnings
Following are specific warnings, precautions, and adverse effects that should be understood by the surgeon and explained to the patient. These warnings do not include all adverse effects that can occur with surgery in general, but are important considerations particular to metallic internal fixation devices. General surgical risks should be explained to the patient prior to surgery.
- IN THE U.S.A., THIS PRODUCT HAS LABELING LIMITATIONS.
- THE SAFETY AND EFFECTIVENESS OF PEDICLE SCREW SPINAL SYSTEMS HAVE BEEN ESTABLISHED ONLY FOR SPINAL CONDITIONS WITH SIGNIFICANT MECHANICAL INSTABILITY OR DEFORMITY REQUIRING FUSION WITH INSTRUMENTATION. These conditions are significant mechanical instability secondary to degenerative spondylolisthesis with objective evidence of neurologic impairment, fracture, dislocation, scoliosis, kyphosis, spinal tumor and failed previous fusion (pseudarthrosis). The safety and effectiveness of these devices for any other conditions is unknown.
- BENEFIT OF SPINAL FUSIONS UTILIZING ANY PEDICLE SCREW FIXATION SYSTEM HAS NOT BEEN ADEQUATELY ESTABLISHED IN PATIENTS WITH STABLE SPINES. Potential risks identified with the use of this device system, which may require additional surgery, include:
- a. Device component fracture
- b. Loss of fixation
- c. Non-union
- d. Fracture of the vertebra
- e. Neurological injury
- f. Vascular or visceral injury
- CORRECT SELECTION OF THE IMPLANT IS EXTREMELY IMPORTANT. The potential for satisfactory fixation is increased by the selection of the proper size, shape and design of the implant. While proper selection can help minimize risks, the size and shape of human bones present limitations on the size, shape, and strength of implants. Metallic internal fixation devices cannot withstand activity levels equal to those placed on normal healthy bone. No implant can be expected to withstand indefinitely the unsupported stress of full weight bearing.
- IMPLANTS CAN BREAK WHEN SUBJECTED TO THE INCREASED LOADING ASSOCIATED WITH DELAYED UNION OR NON-UNION. Internal fixation appliances are load sharing devices which are used to obtain an alignment until normal healing occurs. If healing is delayed or does not occur, the implant may eventually break due to metal fatigue. The degree or success of union, loads produced by weight bearing, and activity levels will, among other conditions, dictate the longevity of the implant. Notches, scratches or bending of the implant during the course of surgery may also contribute to early failure. Patients should be fully informed of the risks of implant failure.
- MIXING METALS CAN CAUSE CORROSION. There are many forms of corrosion damage and several of these occur on metals surgically implanted in humans. General or uniform corrosion is present on all implanted metals and alloys. The rate of corrosive attack on metal implant devices is usually very low due to the presence of passive surface films. Dissimilar metals in contact, such as titanium and stainless steel, accelerate the corrosion process of stainless steel and more rapid attack occurs. The presence of corrosion compounds released into the body system will also increase. Internal fixation devices, such as rods, hooks, wires, etc. which come into contact with other metal objects, must be made from like or compatible metals.
- PATIENT SELECTION. In selecting patients for internal fixation devices, the following factors can be of extreme importance to the eventual success of the procedure:
- The patient’s weight. An overweight or obese patient can produce loads on the device that can lead to failure of the appliance and the operation.
- The patient’s occupation or activity. If the patient is involved in an occupationor activity that includes substantial walking, running, lifting or muscle strain, the resultant forces can cause failure of the device.
- A condition of senility, mental illness, alcoholism, or drug abuse. These conditions, among others, may cause the patient to ignore certain necessary limitations and precautions in the use of the appliance, leading to implant failure or other complications.
- Certain degenerative diseases. In some cases, the progression of degenerative disease may be so advanced at the time of implantation that it may substantially decrease the expected useful life of the appliance. For such cases, orthopaedic devices can only be considered a delaying technique or temporary relief.
- Foreign body sensitivity. Where material sensitivity is suspected, appropriate tests should be made prior to material selection or implantation.
- Smoking. Patients who smoke have been observed to experience higher rates of pseudarthrosis following surgical procedures where bone graft is used.
Precautions
- THE IMPLANTATION OF PEDICLE SCREW SPINAL SYSTEMS SHOULD BE PERFORMED ONLY BY EXPERIENCED SURGEONS WITH SPECIFIC TRAINING IN THE USE OF THIS PEDICLE SCREW SPINAL SYSTEM BECAUSE THIS IS A TECHNICALLY DEMANDING PROCEDURE PRESENTING A RISK OF SERIOUS INJURY TO THE PATIENT.
- SURGICAL IMPLANTS MUST NEVER BE REUSED. An explanted metal implant should never be re-implanted. Even though the device appears undamaged, it may have small defects and internal stress patterns that may lead to early breakage. Additional risks associated with re-use of single use devices include:
- Mechanical malfunction
- Transmission of infectious agents
- CORRECT HANDLING OF THE IMPLANT IS EXTREMELY IMPORTANT. Contouring of the metal implants should only be performed with proper equipment. The operating surgeon should avoid any notching, scratching or reverse bending of the devices when contouring. Alterations will produce defects in surface finish and internal stresses which may become the focal point for eventual breakage of the implant. Bending of screws will significantly decrease fatigue life and may cause failure.
- REMOVAL OF THE IMPLANT AFTER HEALING. Metallic implants can loosen, fracture, corrode, migrate, and possibly increase the risk of infection, cause pain, or stress shield bone even after healing, particularly in young, active patients. The surgeon should carefully weigh the risk versus benefits when deciding whether to remove the implant. Implant removal should be followed by adequate postoperative management to avoid refracture. If the patient is older and has a low activity level, the surgeon may choose not to remove implant thus eliminating the risk involved with a second surgery.
- ADEQUATELY INSTRUCT THE PATIENT. Postoperative care and the patient’s ability and willingness to follow instructions are one of the most important aspects of successful bone healing. The patient must be made aware of the limitations of the implant and that physical activity and full weight bearing have been implicated in bending or fracture. The patient should understand that a metallic implant is not as strong as normal, healthy bone and will fracture if excessive demands are placed on it in the absence of complete bone healing. An active, debilitated, or demented patient who cannot properly use weight- supporting devices may be particularly at risk during postoperative rehabilitation.
- PART NUMBER 3357-1 IS NOT TORQUE LIMITING.
- The DEVICE has not been evaluated for safety and compatibility in the MR environment.The DEVICE has not been tested for heating or migration in the MR environment.
Possible Adverse Effects
- Non-union, delayed union.
- Bending or fracture of implant. Fraying, kinking, loosening, bending or breaking of any or all of the cable implant components.
- Loosening of the implant.
- Metal sensitivity or allergic reaction to a foreign body.
- Infection.
- Decrease in bone density due to stress shielding.
- Pain, discomfort, or abnormal sensations due to the presence of the device.
- Loss of proper spinal curvature, correction height and/or reduction.
- Cable cutting through soft osteoporotic, osteogenic or cancellous bone.
- Vascular and/or nerve damage due to surgical trauma or presence of the device. Neurological difficulties including bowel and/or bladder dysfunction, impotence, retrograde ejaculation and paraesthesia.
- Bursitis.
- Dural leak.
- Paralysis.
- Death.
- Erosion of blood vessels due to the proximity of the device, leading to hemorrhage and/or death.