Product Description
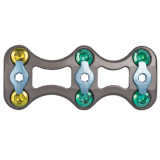
This innovative cervical plate system is designed for anterior interbody screw fixation of the cervical spine. The inVIZiaSystem features direct visualization of implant placement and screw locking for ease of use. With its generous graft window, low profile, simple locking mechanism, narrow waist, and aggressive self-drilling screws, it is a complete solution in one user-friendly spinal implant.
Features
Device Description
The inViZia Anterior Cervical Plate System consists of:
- Cervical plates
- Locking caps
- Fixed and Variable Angle Bone Screws (these are the same bone screws used in the Trinica® Anterior Cervical Plate System)
- Instrumentation necessary for implantation of the system
Indications
The inViZia™ Anterior Cervical Plate System is designed for anterior interbody screw fixation of the cervical spine at levels C2-T1. The inViZia Anterior Cervical Plate System is indicated for use in the temporary stabilization of the anterior spine during the development of cervical spinal fusions in patients with degenerative disc disease (as defined by neck pain of discogenic origin with degeneration of the disc confirmed by patient history and radiographic studies), trauma (including fractures), tumors, deformity (defined as kyphosis, lordosis or scoliosis), pseudoarthrosis and/or failed previous fusions.
WARNING: This device is not approved for screw attachment to the posterior elements (pedicles) of the cervical, thoracic, or lumbar spine.
Contraindications
Contraindications for use of the inViZia Anterior Cervical Plate System include:
- Overt infection or distant foci of infections
- Local inflammation, with or without fever or leukocytosis
- Pregnancy
- Diseases or conditions other than those specifically described in the Indications section
- Use in the posterior elements (pedicles) of the cervical, thoracic, or lumbar vertebrae
- Where attempted correction exceeds the limits of physiological conditions
- Uncooperative patient or patient with neurologic disorders rendering the patient incapable of following instructions
- Metabolic disorders that may impair bone formation
- Inadequate bone stock to support the device
- Inability to restrict high activity level
- Obesity
- Poor prognosis for good wound healing (e.g., decubitis ulcer, end-stage diabetes, severe protein deficiency and/or malnutrition)
Warnings
Some metals, polymers, chemicals, and other materials utilized with orthopedic implants have been known to cause cancer and other adverse body reactions, or reports in the literature have suggested such causation. Any factor that causes chronic damage to tissues may be oncogenic. Cancer can metastasize from soft tissue sites (lung, breast, digestive system, and others) to bone, including areas adjacent to implants, or it can be seeded to these locations during operative and diagnostic procedures (such as biopsies). Paget’s disease has been reported to progress to cancer; surgical candidates suffering from this disease should be warned accordingly.
Implantation foreign material in tissues can elicit an inflammatory reaction. Current literature suggests that wear debris (including metal, polyethylene, ceramic, and cement particles) can initiate the process of histiocytic granuloma formation and consequent osteolysis and loosening.
Metal sensitivity has been reported following exposure to orthopedic implants. The most common metallic sensitivities (nickel, cobalt, and chromium) are present in medical grade stainless steel and cobalt-chrome alloys.
The inViZia Anterior Cervical Plate System is a temporary internal fixation device. Internal fixation devices are designed to stabilize the operative site during the normal healing process. After healing occurs, these devices serve no functional purpose and must be removed. Implant removal should be followed by adequate postoperative management to avoid fracture or refracture.
Precautions
The inViZia Anterior Cervical Plate System instrumentation should only be used after the surgeon has had adequate training in this method of fixation and has become thoroughly knowledgeable about the spinal anatomy and biomechanics. A surgical technique for the inViZia Anterior Cervical Plate System is available upon request. This technique is not a substitute for training and is for general informational purposes only.
The inViZia System uses Trinica System bone screws. Components from other anterior cervical plating systems, however, should not be used with the inViZia System because compatibility has not been established.
Do not use implants made from dissimilar metals (such as cobalt chromium-molybdenum alloy or stainless steel) in contact with components of the inViZia Anterior Cervical Plate System; otherwise, galvanic corrosion may occur.
If contouring of the implant is necessary for optimal fit, the contouring should be gradual and avoid any notching or scratching of the implant(s) surface. The plates must not be repeatedly or excessively bent. Do not reverse bend the plate.
All implants and some instruments are intended for single use only; refer to the product label to determine if the instrument is intended for single use only. Single use devices should not be re-used. Possible risks associated with re-use of single use devices include:
- Mechanical malfunction
- Transmission of infectious agents
Adverse Effects
Complications and adverse reactions have been reported with the use of similar spinal instrumentation systems. These adverse effects, including the possibility of death, should be discussed with the patient prior to surgery.
Possible neurologic operative/postoperative adverse reactions that may require medical or surgical intervention(e.g., implant removal with or without re-instrumentation) include:
- Paralysis, complete or incomplete. Delayed onset has occurred even when evoked potential was unaffected during surgery
- Dural tear leading to cerebrospinal fluid fistula or pseudo meningocele
- Other spinal cord injuries not otherwise described due to positioning of the spinal attachment device
- Laminar erosion
- Epidural bleeding
- Abnormal sensations
- Radiculopathy
- Loosening, bending, breaking, disassembly, and/or migration of the components
- Collapse of a fracture and/or fusion site
- Device failure
- Corrosion at the screw/locking cap interface contributing to breakage, and/or pseudoarthrosis
- Discomfort or pain, soft tissue erosion, or protrusion due to prominent implanted hardware
- Attachment device pullout, especially with short constructs and osteoporotic bone
- Implant or graft extrusion through the skin
- Postural deformities, pain, skin breakdown, or residual neural compression due to kyphosis or lordosis occurring at the top of the segment being instrumented
- Bone loss or fracture due to stress shielding
- Foreign body reaction to the device including tumor formation, autoimmune disease, metallosis, and/or scarring
- Non-union or pseudoarthrosis
- Cessation of growth at the fusion site
- Discitis, arachnoiditis, and/or other types of inflammation
- Hemothorax
- Deep vein thrombosis, thrombophlebitis, and/or pulmonary embolism that may be fatal; may be due to patient position and/or length of the surgical procedure
- Decubitus ulcer
- Wound infection, deep or superficial, which may require implant removal and/or other medical interventions
- Wound dehiscence, delayed wound healing, or hematoma
- Pain, possibly severe in nature
- Urinary tract infection
- Blood vessel damage and/or blood loss or hemorrhage
- Fracture(s) of the bone
- Gastrointestinal, urological, and/or reproductive system compromise including sterility, impotency, and/or loss of consortium
- Bone graft donor site pain
- Inability to resume activities of normal daily living